
In the second project showcase, highlighting impactful studies we’ve delivered as part of our 60th anniversary series, we revisit an important study on patient escalation under pandemic pressures, which informed the Covid 19 Inquiry.
During the COVID-19 pandemic, healthcare systems faced unprecedented strain, significantly impacting healthcare professionals’ ability to escalate patient care. To understand these critical challenges, the UK Covid-19 Inquiry commissioned us to deliver a comprehensive survey of over 1,500 healthcare professionals (HCPs). The study revealed that over half of HCPs (58%) were unable to escalate care due to resource shortages, primarily a lack of beds and staff. These findings highlighted the immense pressures, the ethical dilemmas faced by staff, and provided crucial insights for enhancing healthcare system resilience and preparedness for future crises.
About the client
The UK Covid-19 Inquiry is an independent public investigation into the UK’s preparedness and response to the pandemic, with the aim of learning lessons for the future. As part of its comprehensive investigation, Module 3 focused on the healthcare systems, including their ability to manage critical care capacity, patient triage, and the role of primary care.
The challenge
The Covid-19 pandemic brought significant strain to healthcare systems globally and prompted rapid, far-reaching changes. In the UK, the NHS experienced considerable pressure as hospitals neared capacity, routine treatments were postponed, and frontline staff faced immense demands. The crisis highlighted existing challenges within healthcare infrastructure and required swift decisions about how care was delivered and prioritised.
The Inquiry wanted to understand the frequency and nature of challenges faced by frontline healthcare professionals in making difficult decisions such as when to call patients an ambulance or admit them to critical care. This included the resources that were lacking, the adequacy of support and guidance, and the impact these situations had on staff wellbeing and values.
We were commissioned by the Inquiry to investigate experiences related to the escalation of care across the 4 nations. The project was carried out under strict legal terms of reference and had to be delivered within a fixed timeframe.
The approach
The research was delivered through an online survey targeting healthcare professionals across the UK. A multi-pronged recruitment strategy was used to ensure a rich and diverse dataset, combining commercial samples with outreach to relevant organisations such as ambulance services. Snowball sampling was also used to expand reach and mitigate recruitment risks, by asking healthcare professionals to encourage colleagues to participate. In total, 1,683 responses were collected.
The team conducted pilot and cognitive testing in a matter of days to ensure the survey had inclusive, clear, and effective language that could capture a variety of experiences across different staff roles. This included critical care doctors and nurses, paramedics, GPs, A&E doctors, and hospital ward doctors. Plus, the survey was adapted in real time based on feedback, for example through adding an option for 999 call handlers to be able to complete the survey.
Our findings were delivered in a visual PowerPoint format, designed with courtroom use and public accessibility in mind.

“It was very difficult and upsetting to leave some sick patients at home due to tightening of criteria for conveyance to A&E. Some of these patients would have deteriorated and died. I understand why it had to happen, but it went against my paramedic values.”
Paramedic
The impact
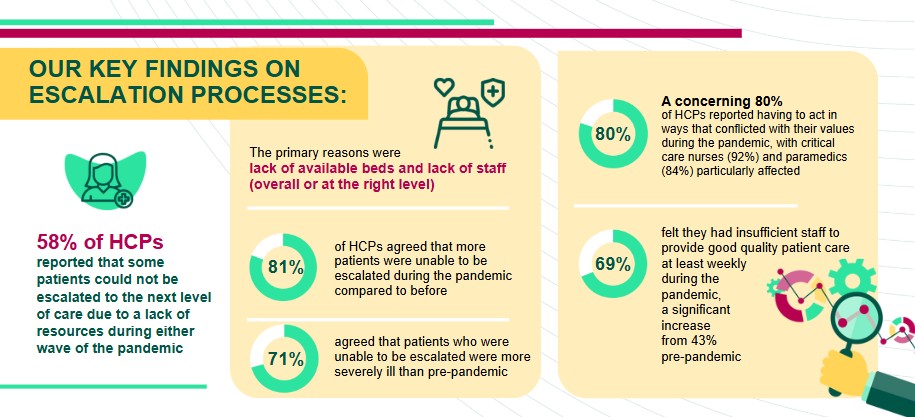
Resource shortages were shown to directly impact care decisions and staff wellbeing. 58% of HCPs reported being unable to escalate patients to the next level of care due to lack of resources during either wave of the virus. This was most common among A&E doctors (71%) and paramedics (62%). And the most cited reasons as barriers were:
- Lack of available beds (including ICU and high-dependency units)
- Lack of staff (overall or at the right level)
- Lack of equipment, ambulance access, and technology
This data highlighted clear systematic vulnerabilities that were worsened by a nationwide health emergency and emphasised the need for future pandemic preparedness. Strategies around boosting bed and staffing capacity, ensuring clear and consistent guidance is widely available, and better supporting staff facing ethical pressures were seen as key to improving processes.
Our evidence was referred to directly in the Module 3 Hearing that took place in September 2024. It formed part of the wider picture that will guide senior political figures in key policy decision making to be better equipped in the future.
“The survey provided a valuable insight into the impact of the pandemic on the care patients received and how this impacted healthcare workers.”
UK Covid-19 Enquiry team
Download case study
To find out more about this project, or how we could help you, contact us at hello@iffresearch.com. You can also download the case study here.